EUS: The Gold Standard in Minimally Invasive Imaging – How Endoscopic Ultrasound Is Revolutionizing Diagnosis and Treatment
EUS: The Gold Standard in Minimally Invasive Imaging – How Endoscopic Ultrasound Is Revolutionizing Diagnosis and Treatment
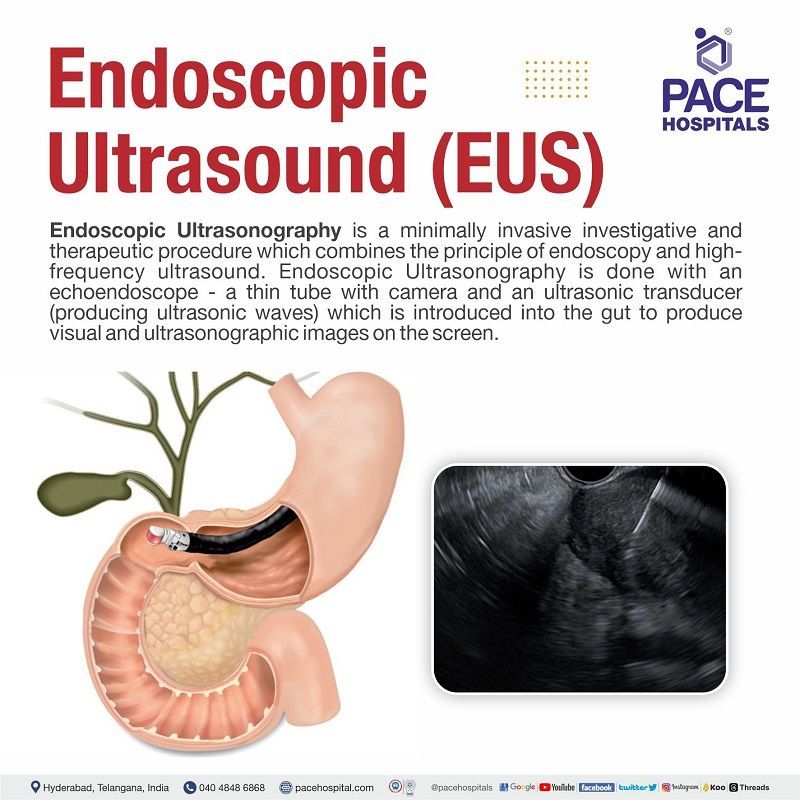
Endoscopic ultrasound (EUS) stands at the forefront of modern diagnostic and interventional medicine, merging endoscopy with high-frequency ultrasound to deliver unparalleled imaging of the gastrointestinal tract and surrounding structures. By combining real-time visualization with fine-needle access, EUS enables physicians to detect, stage, and treat diseases with remarkable precision—often reducing the need for open surgery. As advanced imaging techniques continue to evolve, EUS has emerged as an indispensable tool in oncology, gastroenterology, and pulmonology, offering a dynamic window into hard-to-reach anatomical regions.
Understanding the Mechanics: How Endoscopic Ultrasound Works
At its core, EUS integrates a flexible endoscope equipped with a miniaturized ultrasound probe. Traditional endoscopy provides light and visual clarity along the esophagus, stomach, and proximal duodenum, while the added ultrasound component generates high-resolution cross-sectional images of adjacent tissues—down to just millimeters in depth. The ultrasound component operates at frequencies between 5 and 20 MHz, far higher than diagnostic ultrasound used in OB-GYN or cardiology, allowing detailed imaging of layers within the gastrointestinal wall and nearby organs such as the pancreas, bile ducts, lymph nodes, and even adjacent mediastinal structures.“EUS allows us to see beyond the visible—visualizing tumor invasion, lymph node status, and vascular anatomy with exquisite clarity,” explains Dr. Elena Marquez, a gastroenterologist specializing in EUS at Johns Hopkins. “It’s not just a picture; it’s a complete roadmap for intervention.”
During EUS, the endoscope is advanced through the posterior esophagus (transgastric), anteriorly via the duodenum (transduodenal), or sometimes via the rectum for pelvic targets.
As the probe emits sound waves and collects returning echoes, a real-time multimedia display reveals layers of the GI wall—mucosa, submucosa, muscle, and subserosa—and adjacent extraluminal structures. This layered imaging supports accurate staging of malignancies, particularly in esophageal, gastric, and pancreatic cancers.
Clinical Applications: From Cancer Detection to Therapies
EUS excels in both diagnostic accuracy and therapeutic utility. Among its key applications is esophagogastric cancer staging.Unlike CT or MRI, EUS directly assesses tumor depth, nodal involvement, and target stomatal status—critical factors in determining whether a patient is a candidate for endoscopic resection (ESG). “With EUS, we can measure tumor penetration into the muscularis propria or detect occult nodal metastases missed by other imaging,” notes Dr. Samuel Kim, an interventional gastroenterologist at Memorial Sloan Kettering.
“This precision guides treatment decisions with unprecedented confidence.” Beyond staging, EUS enables fine-needle aspiration (FNA) with near-real-time guidance. This technique allows collection of tissue or fluid samples from suspicious lesions—such as pancreatic cysts, lymph nodes, or thyroid nodules extending into the neck—using a thin needle passing through the endoscopic channel or a separate fine-gauge needle inserted via the EUS gate. FNA guided by EUS achieves diagnostic sensitivity exceeding 90% in select cases, rivaling open biopsy while minimizing risk and discomfort.
Therapeutically, EUS has paved the way for EUS-guided fine-needle biopsy (EUFNB) and EUS-guided celiac plexus block (EUS-GCPB). The celiac plexus, a nerve bundle controlling abdominal pain in pancreatic cancer patients, is effectively targeted via EUS to deliver targeted pain relief with minimal systemic side effects. Similarly, EUS founders & seer techniques are increasingly used to manage biliary or pancreatic ductal obstructions, replacing older surgical approaches with less invasive alternatives.
Expanding Frontiers: EUS in Specialized Domains
Historically confined to the upper GI tract, EUS is rapidly expanding into adjacent specialties.Transventricular EUS (TV-EUS), for example, enables imaging of cardiac structures from inside the esophagus, offering a less invasive alternative to transesophageal echocardiography (TEE) in specific cardiac evaluations. Meanwhile, endorespiratory EUS (ER-EUS) improves lung lesion visualization by synchronizing breath-hold imaging with respiratory gating, enhancing detection of peripheral pulmonary nodules and lymphadenopathy. In biliary and pancreatic disease, EUS remains central for confirming malignancy, guiding drainage of infected pancreatic pseudocysts, and facilitating targeted ablation of unresectable tumors.
Novel techniques like EUS-guided percutaneous transhepatic or transgastric biopsy (EUP-TBx) provide safe diagnostic access to deep lesions, expanding endoscopic reach beyond the GI mucosa.
The integration of contrast-enhanced EUS (CE-EUS) further enhances tissue characterization, distinguishing benign from malignant lesions based on vascularity patterns. Exogenous microbubbles, injected intravenously, highlight perfusion dynamics in real time—supporting earlier, more accurate diagnoses and reducing diagnostic ambiguity.
Advantages and Limitations: Weighing EUS in Clinical Practice
EUS offers profound clinical benefits.Its high spatial resolution, intuitive 3D navigation, and real-time feedback make it uniquely suited for targeted interventions. Patients typically undergo EUS under moderate sedation, with recovery taking hours—not days—compared to surgery. The time and cost savings alone make EUS a compelling choice in optimized healthcare systems.
However, challenges persist. The procedure requires specialized training: accurate needle placement demands expertise to avoid complications such as perforation, bleeding, or pancreatitis—though the risk, when performed by experienced practitioners, remains low. Equipment costs, maintenance, and staff training represent significant investment barriers for smaller facilities.
Moreover, EUS is limited by anatomical constraints. Deep-seated tumors or distant metastases may elude optimal imaging, and patient factors such as severe obesity, severe acid reflux, or prior abdominal surgery can reduce visibility. Nevertheless, ongoing advances in probe design, imaging algorithms, and training methodologies continue to expand its accessibility and safety.
The Future of EUS: Innovation Meets Precision Medicine
The trajectory of EUS reflects broader trends in medicine: minimally invasive, image-driven, patient-centered care. Emerging technologies—such as fusion EUS with MRI or CT for enhanced pre-procedural planning, artificial intelligence for automated layer analysis, and micro-robotic EUS platforms for remote manipulation—are poised to redefine diagnostic thresholds and therapeutic possibilities. As research deepens understanding of disease biology, EUS will increasingly serve as both a diagnostic lens and therapeutic platform.Integration with molecular imaging, liquid biopsy, and targeted drug delivery holds promise for personalized treatment pathways informed by real-time, tissue-specific data. What makes EUS truly transformative is its dual role: it reveals anatomy with microscopic clarity and empowers clinicians to intervene with surgical precision—all within a single, patient-friendly procedure. In an era where early detection and targeted therapy define outcomes, EUS stands not just as a tool, but as a cornerstone of modern clinical practice.
With ongoing innovation and expanding clinical adoption, endoscopic ultrasound continues to bridge gaps in diagnosis and treatment, offering patients a safer, more accurate path forward. As technology evolves, so too does the frontier of what’s possible in minimally invasive care—anchored by EUS as both explorer and healer.


Related Post

PT Denso Manufacturing Indonesia: Engine Driving Innovation in Automotive Component Excellence

Decoding 18:00: The Precise Moment Time Reveals
From Plaster Chains to Feasting Tables: The Surprising Legacy of Pigs in the Parlor

Starburst Your Coffee: The Ultimate Guide to Grande Drinks Your Size at Starbucks

