Impaired Skin Integrity Nursing Diagnosis: The Silent Threat Every Nurse Must Recognize
Impaired Skin Integrity Nursing Diagnosis: The Silent Threat Every Nurse Must Recognize
Every patient hour spent in preventable skin breakdown reflects a gap in care—yet impaired skin integrity remains a common, often underestimated nursing challenge that demands vigilance, protocol, and empathy. Nursing diagnoses centered on impaired skin integrity are not merely clinical labels; they represent critical opportunities to intervene before pressure injuries escalate into life-threatening wounds. With rising rates of hospital-acquired pressure injuries and ulcerations, understanding the underlying causes, risk factors, and evidence-based prevention strategies is essential for every frontline nurse.
Impaired skin integrity refers to any breach in the skin’s natural barrier, including deterioration of tissue integrity of the skin, providing “a vulnerable window where healing depends on early detection and precise intervention.” This condition spans a spectrum—from simple erythema to deep ulcers—and primarily affects immobile, elderly, or chronically ill patients. Despite its preventable nature, recent studies indicate that pressure injuries affect over 2.5 million patients annually in U.S. hospitals, with infection and delayed healing adding significant morbidity and healthcare costs.
Key Risk Factors: Identifying Patients at High Vulnerability
Several well-documented risk factors elevate a patient’s susceptibility to skin breakdown, demanding thorough assessment during initial evaluations and ongoing monitoring.The most significant contributors include: - **Immobility**: Prolonged pressure reduces blood flow, accelerating tissue damage. Bedridden or wheelchair-bound patients lose the ability to shift weight, making them prone to localized ischemia. - **Poor Nutrition**: Deficiencies in protein, vitamins (especially A and C), and hydration impair collagen synthesis and wound repair.
Malnourished patients often exhibit fragile, dry skin that breaks more easily. - **Incontinence**: Prolonged exposure to moisture from urine or feces disrupts the skin’s protective barrier, fostering maceration and increases susceptibility to infection. - **Medically Related Conditions**: Neurological impairments (e.g., spinal cord injury), diabetes mellitus, and vascular disease compromise circulation and sensation, weakening skin resilience.
- **Advanced Age**: Senescent skin loses elasticity and subcutaneous fat, increasing fragility and slowing regeneration. Age-related declines in immune function further limit healing resilience. “Skin is our body’s first line of defense,” says clinical nurse specialist Dr.
Elena Marquez. “When risk factors converge, even minor pressure or friction becomes dangerous—early recognition is survival.”
Clinical Signs and Staging: Recognizing Impaired Skin Integrity Early
Timely identification hinges on recognizing subtle changes before full-thickness injury occurs. Nurses must conduct thorough skin assessments on a regular schedule, using standardized tools like the Braden Scale to evaluate risk.The wound intensity progresses through defined stages, each demanding specific interventions: - **Stage 1**: Intact skin with non-blanchable redness—early warning of compromised perfusion. No breaking of the skin; preventive measures are urgent. - **Stage 2**: Partial-thickness loss with intact or ruptured skin; often appears as a superficial open area resembling a blister.
Requires stacking dressings and off-loading pressure. - **Stage 3**: Full-thickness ulcer extending through dermis into subcutaneous tissue, without bone, tendon, or muscle exposed. Risk of deep infection and systemic spread rises significantly.
- **Stage 4 and Beyond**: Dead tissue (eschar), fascia, muscle, or bone involvement; often associated with necrosis and odor. May indicate prolonged neglect and require complex wound care or surgical debridement. Monitoring for pressure points—such as sacrum, heels, and elbows—is vital.
Nurses should document changes meticulously, enabling early intervention before irreversible damage occurs.
Evidence-Based Prevention and Intervention Strategies
The cornerstone of managing impaired skin integrity lies not in treatment—but in prevention. The nursing role is proactive, blending clinical expertise with patient-centered strategies.Key interventions include: - **Risk Assessment using Braden Scale**: Systematically evaluating sensory perception, moisture, activity, mobility, nutrition, and friction/friction via the Braden scale enables targeted surveillance. - **Repositioning Protocols**: Regular turning schedules—every 2 hours for bedridden patients, or 15-minute intervals when repositioning—are foundational to off-loading pressure. Advanced devices such as alternating pressure mattresses and low-air-loss beds further reduce risk.
- Skin Protection and Hydration**: Barrier creams (e.g., zinc oxide or hydrocolloids) shield vulnerable areas, while frequent gentle cleansing and use of pH-neutral, moisturizing products maintain skin integrity. - Nutritional Optimization: Collaborating with dietitians to ensure adequate protein intake (1.2–2.0 g/kg/day), vitamin C and zinc levels supports tissue strength and healing. Hydration remains equally critical to skin resilience.
- Incontinence Management: Immediate cleaning with pH-balanced wipes, use of barrier




Related Post
Genshin Impact Keeps Logging You Out — Here’s Why the Bug Persists and What Players Are Facing
Elwood Indiana Funeral Homes: Confronting the Uncomfortable Questions We Can’t Avoid
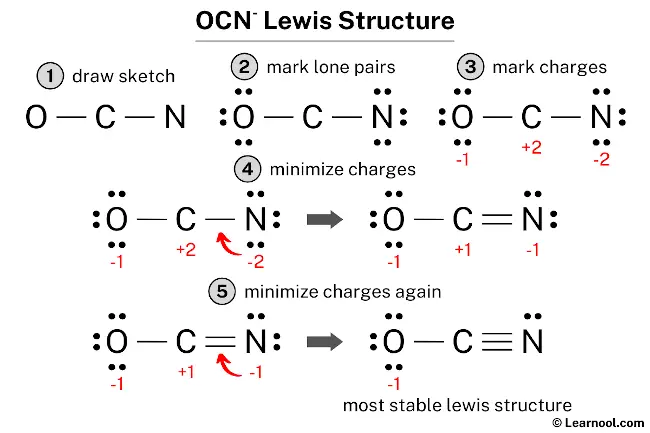
Decoding Chemistry’s Blueprint: Mastering the Ocn-Lewis Structure for Precise Bonding Insights

