Specimen Icteric: The Clinical Key to Jaundice Diagnosis
Specimen Icteric: The Clinical Key to Jaundice Diagnosis
When jaundice first appears—yellowing of the skin and mucous membranes—the body speaks a language of tangible signs, with Specimen Icteric emerging as the definitive clinical indicator. This term, derived from the Latin *ictericus* and rooted in medical tradition, represents not just a visual symptom, but a critical diagnostic focal point in diagnosing and managing liver and hemolytic disorders. Specimen Icteric is more than a clinical observation; it is a linchpin in identifying underlying pathology, guiding treatment decisions, and monitoring disease progression.
As hepatology advances, the precise recognition of this phenomenon remains indispensable across emergency and primary care settings.
Specimen Icteric manifests as a characteristic hyperbilirubinemia-induced hue shift—most prominently in the sclera, conjunctiva, oral mucosa, and nail beds—reflecting elevated levels of unconjugated bilirubin in the bloodstream. Unlike secondary or benign pigmentation that fades with time or hydration, this jauice color is pathognomonic, signaling hepatic dysfunction, impaired bilirubin metabolism, or red blood cell breakdown.
Its diagnostic significance lies in its specificity: while other conditions may mimic jaundice—such as liver failure, anemia, or hemolysis—the presence and pattern of Specimen Icteric anchor clinicians to a core etiology. “In practice, detecting Specimen Icteric is often the first step toward unraveling the root cause of jaundice,” notes Dr. Elena Marquez, a clinical hepatologist at the Institute for Liver Research.
“It transforms ambiguity into actionable insight.”
Pathophysiology Underlying Specimen Icteric
To understand Specimen Icteric, one must first trace its metabolic roots. Bilirubin, a byproduct of hemoglobin degradation, enters the bloodstream primarily as unconjugated (indirect) bilirubin, bound to albumin. The liver then conjugates it to water-soluble forms for excretion into bile.When this cascade falters—due to hepatocellular injury, bile duct obstruction, hemolysis, or inherited metabolic defects—bilirubin accumulates in plasma. Unconjugated bilirubin, fat-soluble and neurotoxic, crosses lipid barriers with ease, rather than through urinary excretion, ultimately depositing in tissues. The sclera’s thin epithelial layer and prominent vascularity render the eyes particularly sensitive to this pigment cascade.
Oral mucosa and skin follow, with the degree of yellowing directly proportional to serum bilirubin concentration. “Specimen Icteric is not merely a surface change,” explains Dr. James Tran, a gastroenterology leader at Regional Medical Center.
“It reflects a systemic metabolic bottleneck—often telltale for cholestasis, hepatitis, or severe hemolytic activity.”
Clinical patterning differentiates Specimen Icteric from other jauice presentations. Whether conjugated (direct) or unconjugated, the color varies subtly: conjugated jaundice often appears more uniformly yellow or amber, while unconjugated—seen in Specimen Icteric—tends toward bright lemon or canary yellow hues, particularly noticeable in dark circles of the eyes. The sclera’s visibility makes it the most reliable site for clinical assessment, with tool-assisted documentation improving diagnostic accuracy.
Point-of-care imaging and digital color analysis now aid objective measurement, reducing subjectivity in detection. Studies show that careful examination of conjunctival pigmentation correlates strongly with serum bilirubin levels, validating Specimen Icteric as a tangible, quantifiable sign.
Clinical Applications and Diagnostic Weight
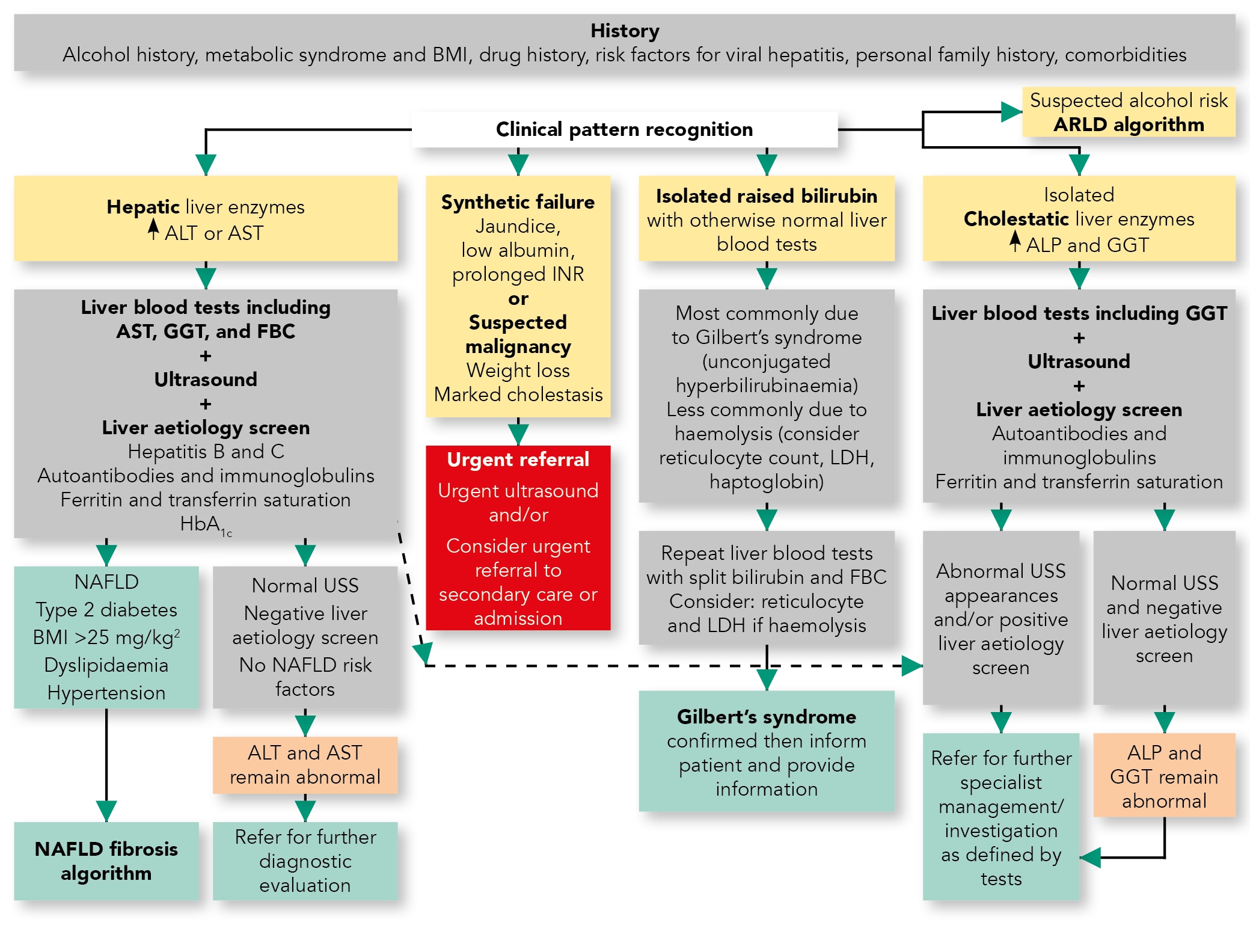
Specimen Icteric’s role in clinical workflows is multifaceted, serving as both a primary clue and a monitor of therapeutic response. In emergency departments, a patient presenting with pronounced yellowing upon eye examination immediately raises suspicion for acute liver injury—whether acute viral hepatitis, drug-induced hepatotoxicity, or obstructive cardiac jaundice.“Patients with rapidly progressing Specimen Icteric often have underlying conditions demanding urgent intervention,” emphasizes Dr. Marquez. Blood tests confirming elevated indirect bilirubin levels strengthen the diagnostic weight, guiding decisions about hospitalization, imaging (like ultrasound or MRI), or referral to hepatology.
In primary care, Specimen Icteric acts as a red flag prompting further evaluation. A pediatrician assessing yellowing of a newborn’s eyes promptly considers hepatobiliary causes like biliary atresia, while an adult presenting with jauice but no fever or abdominal pain warrants investigation into hemolytic disorders or hepatocellular damage. >“The presence of Specimen Icteric shortens diagnostic uncertainty,” says Dr.
Tran. “It’s the clinician’s first clue in a sequence of tests and interventions.” Beyond initial diagnosis, Specimen Icteric’s evolution tracks disease dynamics. In viral hepatitis, its intensity often wanes with antiviral therapy or resolves at recovery.
Conversely, persistent or worsening yellowing signals renal failure, Wilson’s disease, or malignancy, prompting tailored management. Longitudinal monitoring via repeated observation of Specimen Icteric helps gauge treatment efficacy—clinicians measure color change over time, correlating subjective findings with laboratory data to refine prognoses.
Differential diagnosis is integral to interpreting Specimen Icteric correctly.
Conditions such as carotenemia (orange pigment from diet), Kupfer-certain diseases (in liver failure), or pigmentation from ocular trauma may mimic yellowing. However, Specimen Icteric distinguishes itself by: - Its association with elevated indirect bilirubin, - Localization predominantly in mucosal surfaces, - Consistency with metabolic derangements rather than dietary or traumatic origin. Laboratory confirmation—via serum bilirubin, liver function tests, and imaging—anchors interpretation and prevents misdiagnosis.
Prognostic Implications and Clinical Utility
The overt appearance of Specimen Icteric carries profound prognostic weight.In acute hepatic injury, timely recognition reduces risk of complications like hepatic encephalopathy or multi-organ failure. In oncology, persistent jauice signals disease progression, compelling urgent oncologic assessment. Public health initiatives emphasize early clinical recognition to improve outcomes, particularly in resource-limited settings where advanced diagnostics may be delayed.
Healthcare providers rely on Specimen Icteric not only for diagnosis but also for communication—accounting for visual cues helps bridge patient-clinician understanding, reinforcing urgency and care continuity. “Patients often connect the yellowing directly to illness,” notes Dr. Marquez.
“This shared observational experience builds trust and motivates adherence.”
Innovations in Detecting and Documenting Specimen Icteric
Technological advances are refining how Specimen Icteric is assessed. Portable dermometers and smartphone-based spectrophotometers now enable standardized color quantification, integrating digital snapshots with algorithm-driven bilirubin estimation. These tools minimize human error, especially in pediatric care where subtle changes matter.Clinical decision support systems alert providers to jaundice patterns matching Specimen Icteric, prompting earlier intervention. Telemedicine platforms increasingly incorporate real-time visual assessment, enhancing diagnostic reach in remote care. “Accurate, objective measurement transforms subjective observation into standardized data,” says Dr.
Tran, underscoring how innovation deepens clinical reliability.
From newborns to adults, Specimen Icteric remains a universal clinical sign—rooted in biochemistry, shaped by physiology, and pivotal in decision-making. What begins as a visible hue in the sclera evolves into a gateway for diagnosis, monitoring, and treatment.
Its enduring relevance underscores a core truth in medicine: sometimes, the simplest findings hold the greatest power.



Related Post

Deion Sanders Kids: The Legacy Live On in the Next Generation

Weatherct Your Ultimate Guide to Connecticut’s Climate: A Deep Dive into the State’s Unique Weather Patterns

