Sympathetic vs. Parasympathetic: The Body’s Internal Balance at War and Harmony
Sympathetic vs. Parasympathetic: The Body’s Internal Balance at War and Harmony
When the human nervous system responds to stress, arousal, or rest, two halves engage in a precise, continuous tug-of-war: the sympathetic and parasympathetic branches of the autonomic nervous system. This dynamic interplay shapes everything from heart rate and digestion to alertness and emotional regulation. Understanding the contrast between these systems reveals not just physiological mechanisms, but the invisible forces guiding how we function day to day — and how chronic imbalance may undermine health.
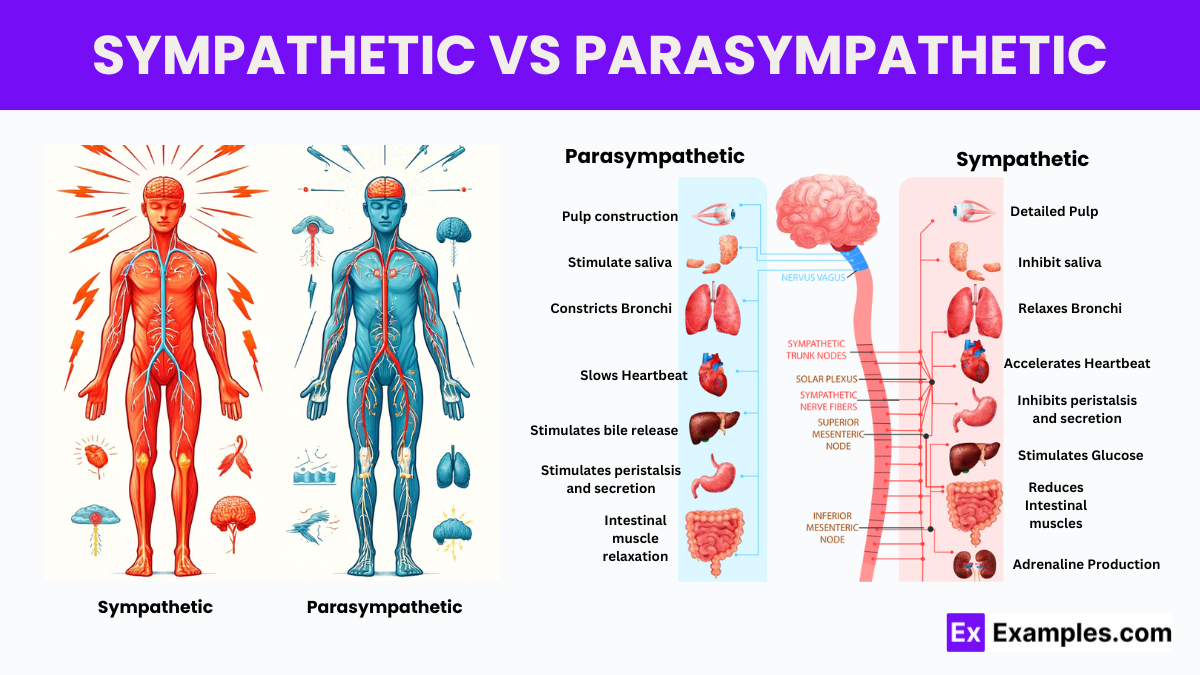
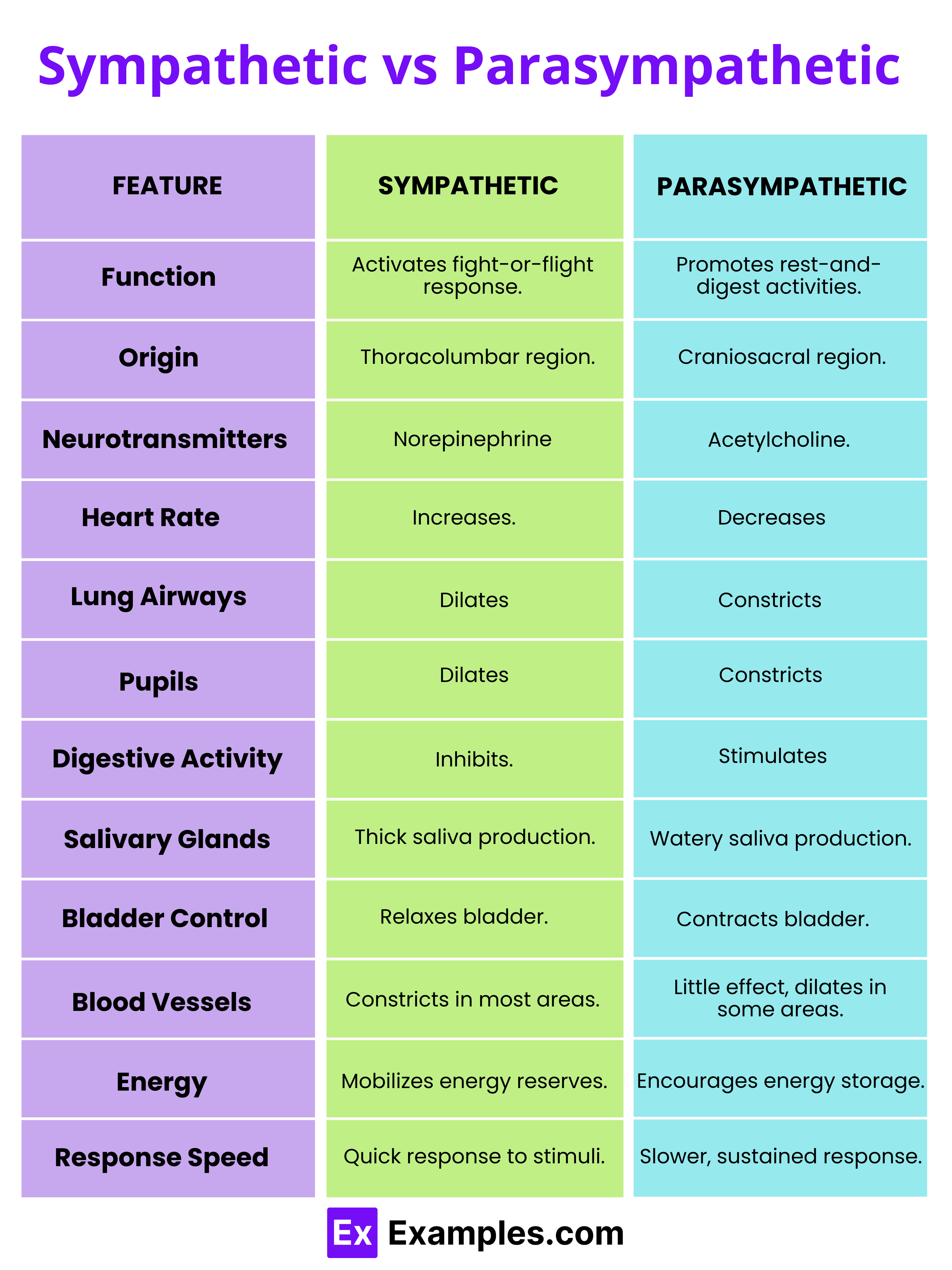
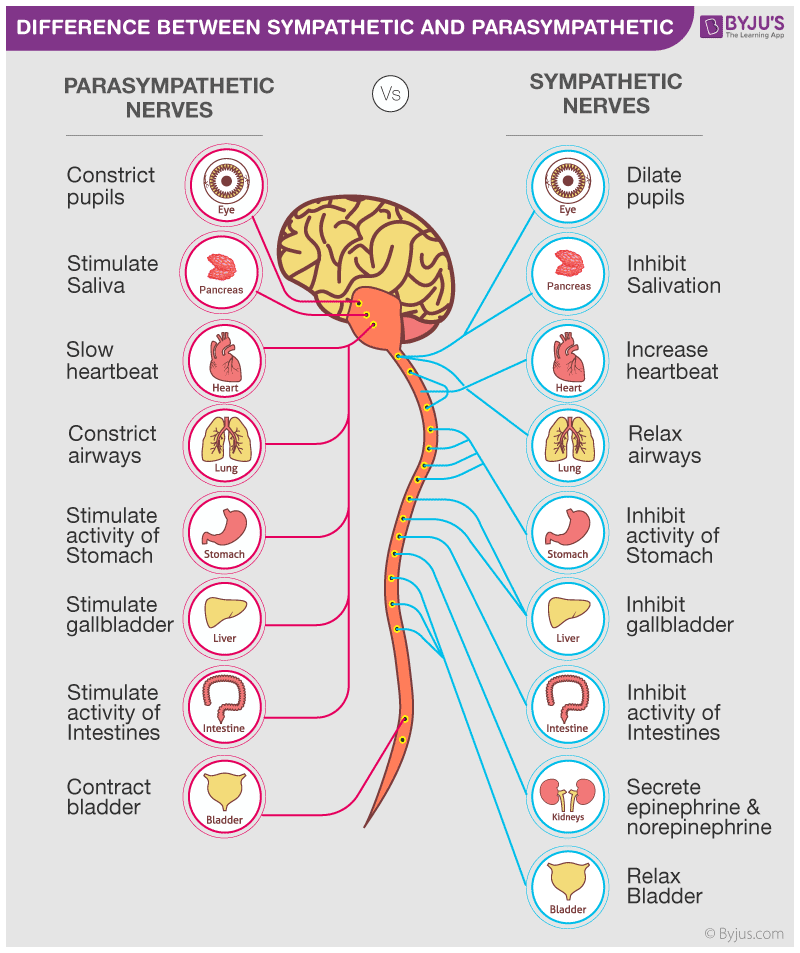
The sympathetic nervous system (SNS), often dubbed the “fight or flight” network, activates the body’s rapid-response mode. Triggered by perceived threats — whether physical danger or psychological stress — it releases adrenaline and noradrenaline, preparing muscles, accelerating the heart, and redirecting blood flow from digestion to extremities. This cascade generates immediate energy and heightened awareness.
In stark contrast, the parasympathetic nervous system (PNS) embodies the “rest and digest” paradigm, promoting calm, conservation, and recovery. It slows heart rate, stimulates digestion, and fosters cellular repair during periods of safety and rest. The fundamental difference lies in their signaling motifs: • Sympathetic arousal triggers rapid, short-lived responses, increasing energy mobilization for acute challenges.
• Parasympathetic activity enables sustained energy efficiency, supporting growth, healing, and mental clarity. This balance—often measured in milliseconds—determines physiological resilience. When the SNS dominates chronically due to stress, anxiety, or lifestyle, the PNS becomes underactive, creating a state of persistent physiological imbalance.
“The body doesn’t distinguish between mental threat and physical danger,” explains Dr. Sarah Lin, a neurophysiologist at Stanford University. “Both trigger the same autonomic cascade—unless consciously redirected.”
How the Sympathetic Nervous System Aggressively Mobilizes Response
Activation of the sympathetic nervous system is a finely tuned physiological cascade.Upon detection of stress—real or imagined—brain regions like the amygdala rapidly signal the hypothalamus, which—via the spinal cord—activates sympathetic neurons. Pulses of adrenaline released from the adrenal medulla flood circulatory pathways, while the adrenal glands secrete cortisol, prolonging the stress response. Key effects include:
- Increased heart rate and blood pressure: Accelerating circulation to critical muscles and organs.
- Dilated airways: Enhancing oxygen intake for peak physical output.
- Glucose release from liver stores: Delivering immediate energy via elevated blood sugar.
- Suppressed non-essential functions: Digestion slows; immune activity dampens temporarily.
Yet, modern life often keeps this system locked in high gear, weakening long-term health.
Parasympathetic System: The Architect of Restorative Equilibrium
Where the sympathetic system prepares for action, the parasympathetic takes charge of conservation and renewal. Comprising cranial nerves (especially cranial nerve X, the vagus) and sacral outflow from the spinal cord, the PNS exerts inhibitory control over stress responses.Its primary role is to restore homeostasis: activating the "rest and digest" sequence by:
- Slowing heart rate and lowering blood pressure: Promoting cardiovascular stability and relaxation.
- Stimulating digestion: Encouraging saliva production, gastric secretion, and peristalsis.
- Supporting metabolic repair: Enhancing insulin sensitivity and nutrient absorption.
- Enhancing cognitive function: Facilitating memory consolidation and emotional regulation via the hippocampus and prefrontal cortex.
“Higher vagal activity correlates with stronger ability to calm the body after stress.”
This balance isn’t static—it fluctuates constantly, adapting to environmental cues. A sudden noisesrals? The SNS fires.
A quiet bathroom after a crisis? The PNS takes over. The body’s mastery lies in its fluid oscillation between activation and restoration, a rhythm so subtle it goes unnoticed—until it’s disrupted.
Imbalances and Their Impact on Health and Performance
Chronic sympathetic dominance disrupts this equilibrium and fuels a range of conditions.Persistent elevation in stress hormones promotes hypertension, insulin resistance, and weakened immunity. Long-term imbalance correlates with anxiety disorders, insomnia, gastrointestinal diseases, and even cardiovascular decline. “When the body stays in fight or flight mode,” warns clinical psychologist Dr.
Elena Torres, “it exhausts physiological reserves and masks deep repair processes.” Conversely, a well-regulated PNS supports resilience. Individuals with strong vagal tone exhibit lower resting heart rates, faster recovery from exertion, and superior emotional regulation. Athletes often train vagal responsiveness through breathwork, leveraging heart rate variability (HRV) as a biomarker of readiness.
In everyday life, the presence of calm moments—mindful pauses, intentional breathing—augments parasympathetic tone, reinforcing long-term wellness.
Practical Pathways to Restore Autonomic Balance
Reclaiming balance between sympathetic and parasympathetic control is both accessible and evidence-based. Key strategies include:- Mindfulness and meditation: Practices like focused breathing stimulate vagus activity and quiet stress signaling.
“Neuroscience confirms breath directly influences the heart rate variability and autonomic switch,” says Dr. Park.
- Physical exercise—especially moderate aerobic activity: Regular movement enhances overall autonomic flexibility, reducing resting SNS tone.
- Quality sleep: Poor sleep amplifies sympathetic drive; consistent, restorative rest recalibrates stress pathways.
- Social connection: Positive interpersonal interactions trigger oxytocin release, which dampens sympathetic activation.
Understanding the dynamic tension between sympathetic and parasympathetic systems illuminates how internal environments shape health. More than a mechanical process, this balance orchestrates every physiological function—from cellular metabolism to emotional stability. In an age of perpetual stimulation, learning to honor both activation and restoration isn’t merely self-care; it’s the cornerstone of lasting vitality.
In the quiet dance between fight or flight and rest and digest, the body's survival hinges on staying poised within the sweet spot of resilience.Mastery of this balance is not reserved for the exceptional athlete or scientist—but belongs to anyone willing to listen to the silent signals coursing through their autonomic nervous system.

Related Post
Freedom Unleashed: How Free Wood Burning Patterns Are Revolutionizing Creative Expression

The Chosen Chaim Potok Pdf: A Profound Exploration of Identity, Intellect, and Faith

Gsf Bandit 1200 S: Redefining Desktop Security with Advanced Hardware-Enabled Privacy
All There Is To Know About Hugh Hefners Son

