The Evolution of HTN in ICD-10: A Critical Watchpoint in Global Hypertension Management
The Evolution of HTN in ICD-10: A Critical Watchpoint in Global Hypertension Management
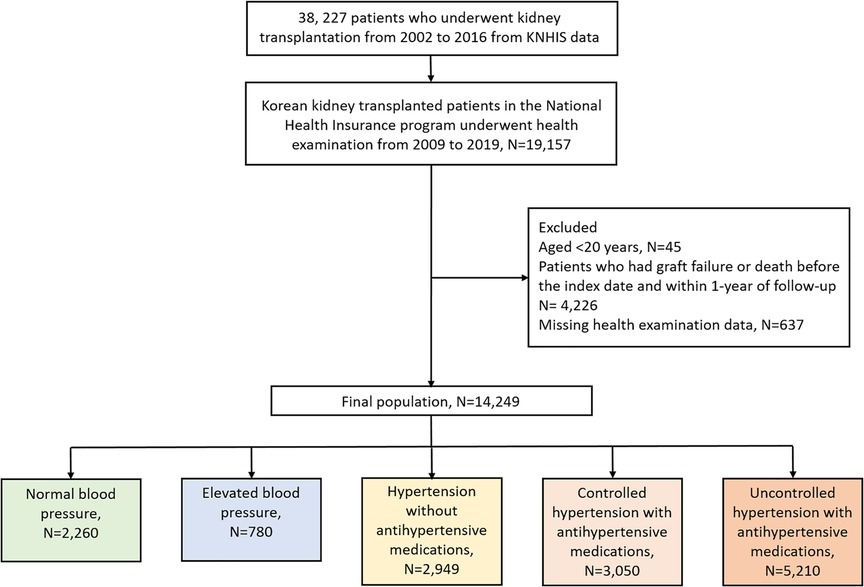
From its formal codification in ICD-10 to its global clinical application, the classification of hypertension—officially known as HTN (Hypertension)—has shaped diagnostics, research, and treatment strategies for decades. Rooted in a century of evolving medical understanding, the inclusion of hypertension in ICD-10 reflects not just a diagnostic label, but a turning point in recognizing cardiovascular disease as a leading public health challenge. This article traces the historical development of HTN within the ICD-10 framework, examines its coding specificity, and evaluates how these standards influence clinical practice and global health monitoring.
The Foundational Codification: HTN in ICD-10’s Birth and Early Implementation
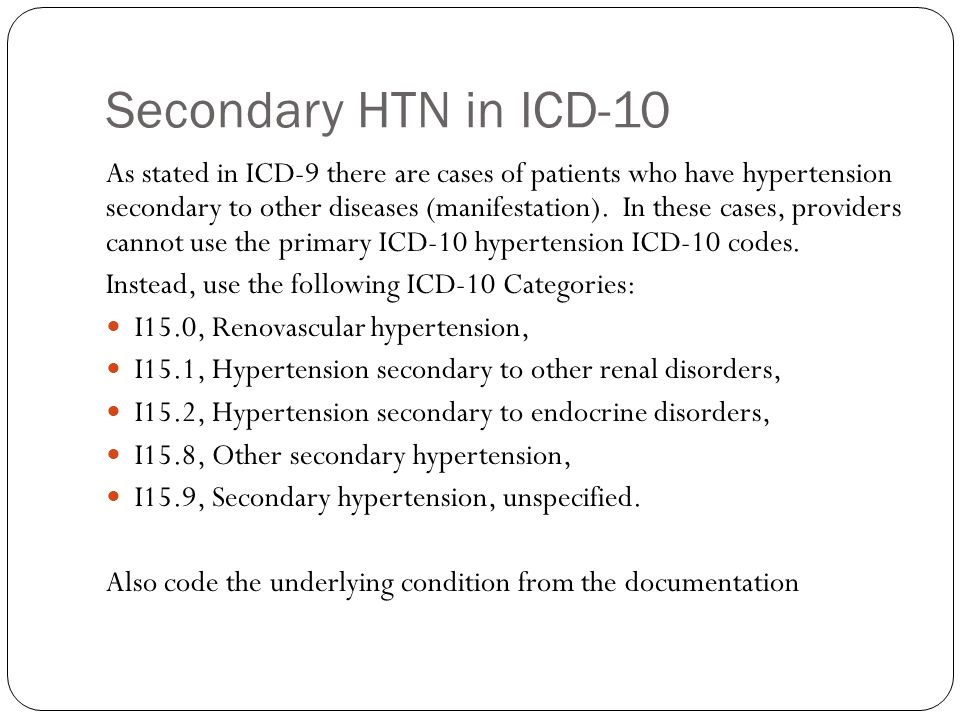
When the International Classification of Diseases, Tenth Revision (ICD-10), published by the World Health Organization (WHO) in 1992, replaced its predecessor ICD-9, hypertension was formally honored with new diagnostic categories.Hypertension itself was split into four distinct entries: - **I10 Hypertension, essential (primary)**: patients with elevated blood pressure with no secondary cause. - **I11 Hypertension, secondary**: hypertension linked to identifiable underlying conditions such as renal disease or endocrine disorders. - **I12 Hypertension with chronic kidney disease**: a subcategory reflecting growing evidence of organ damage interplay.
- **I16 Hypertension with co-morbid conditions**: capturing complex presentations relevant to real-world patient profiles. “This level of granularity was revolutionary,” notes Dr. Elena Marquez, a medical historian specializing in clinical diagnostics.
“For the first time, clinicians had a standardized language that acknowledged not just hypertension’s presence, but its diverse manifestations and complications.” The inclusion of I10 as the core code established HTN as a principal diagnostic condition, enabling consistent reporting across health systems. In a pivotal WHO statement, ICD-10 documentation declared: “Accurate coding of hypertension is not merely administrative—it’s a vital tool for tracking cardiovascular risk and evaluating treatment outcomes.” The deliberate separation of primary, secondary, and secondary-complication forms allowed healthcare providers to stratify risk, tailor interventions, and enroll patients in preventive care pathways more effectively.
With ICD-10, hypertension moved beyond vague clinical impressions to a quantifiable, universally recognized entity.
This shift empowered epidemiologists to track incidence, monitor treatment adherence, and inform policy—transforming HTN from a siloed diagnosis into a measurable public health priority.
Coding Precision: ICD-10’s Structural Nuances and Clinical Relevance
The ICD-10 código structure for hypertension reflects a meticulous effort to balance clinical detail with global applicability. Each code specific to HTN includes definitional parameters that guide accurate diagnosis and billing: - **I10 (Essential hypertension)**: defined by systolic BP ≥130 mmHg or diastolic ≥80 mmHg in adults without known secondary causes, emphasizing primary etiology. - **I11 (Secondary hypertension)**: assigned when hypertension arises from defined secondary conditions, signaling underlying pathology.- **I12 (Hypertension with renal comorbidity)**: captures blood pressure in patients with chronic kidney disease, integrating multi-s


Related Post
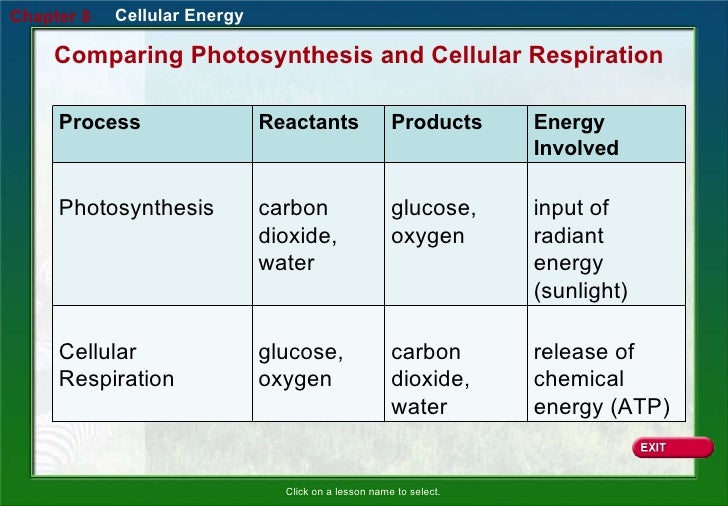
Power at the Cellular Level: The Core Reactants and Products of Respiration
WW3 Nightmare Is Coming: America Must Prepare for the Unthinkable, as Warned by Albert Pike’s Warnings
The Ree Marie Leak What Really Happened Experts Reveal All

